Radiographic Case Review: Chronic Lower Airway Disease in a Young Cat
Meet the patient: a young Russian Blue mix presenting with a persistent cough.
Clinical Presentation:
A 2-year-old male neutered Russian Blue mix cat presented with a two- to three-week history of non-productive coughing. Physical examination revealed no respiratory distress and normal cardiac auscultation.
The only gastrointestinal sign was a single episode of vomiting. Given the clinical course and signalment, chronic respiratory disease was suspected. Thoracic radiography was undertaken to evaluate pulmonary architecture and exclude cardiac or infectious etiologies.
Radiographic Assessment:
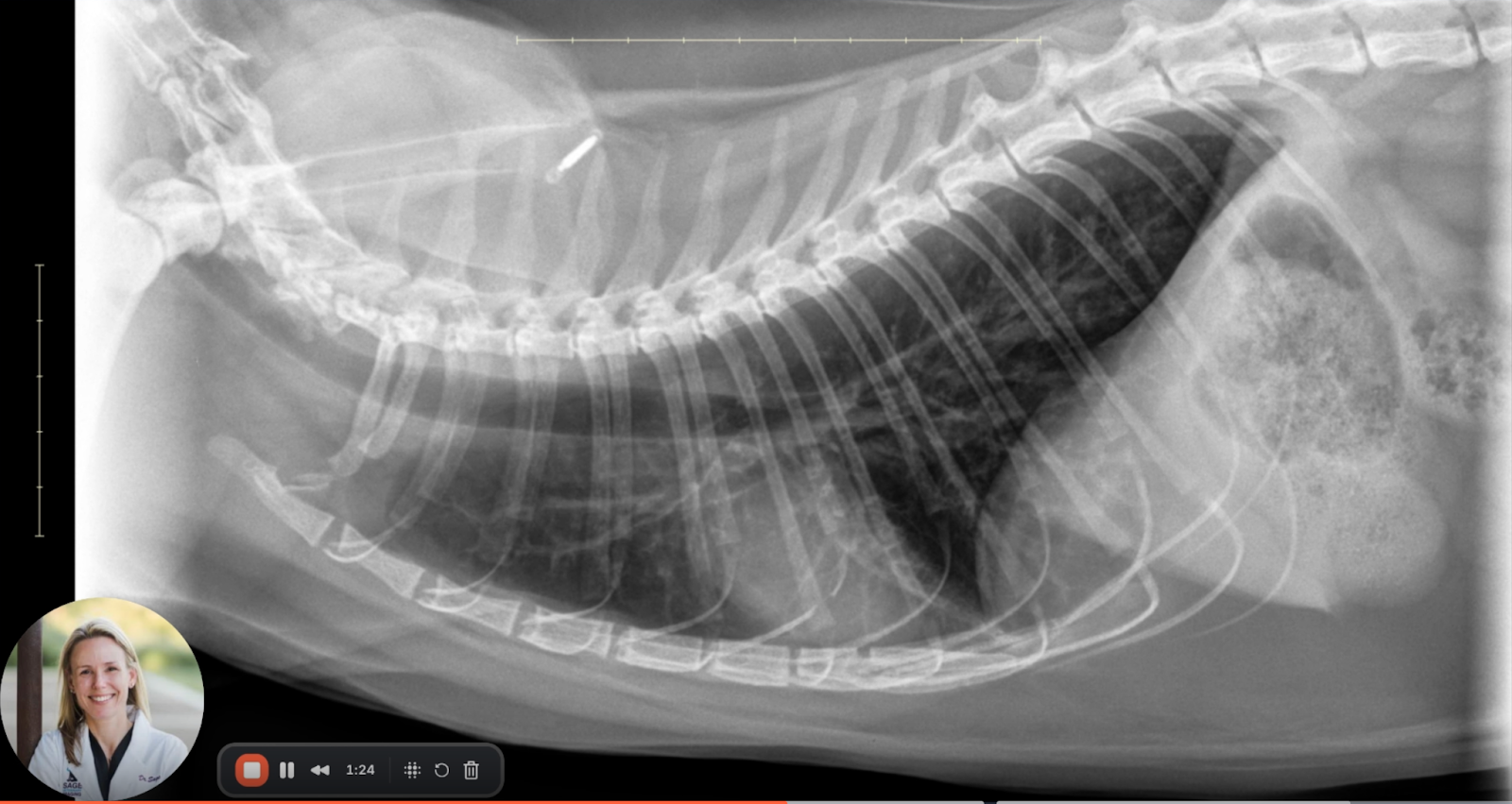
Image 1: Right Lateral View
Cardiac Silhouette: Normal in size and shape with no radiographic signs of cardiomegaly, pulmonary venous congestion, or right heart enlargement.
Pulmonary Parenchyma: A generalized bronchial pattern is evident throughout both lung fields. Bronchial wall thickening is pronounced, producing characteristic “railroad track” signs in longitudinal sections and “donut ring” appearances in transverse sections—radiographic hallmarks of chronic bronchial inflammation.
Pulmonary Inflation: Notable hyperinflation is present. The diaphragm appears flattened, and intercostal spaces are widened, indicating expiratory air trapping and increased lung volume.
Tracheal Morphology: There is dilation of the intrathoracic trachea relative to the cervical portion, a finding consistent with obstructive lower airway disease and reduced expiratory airflow.
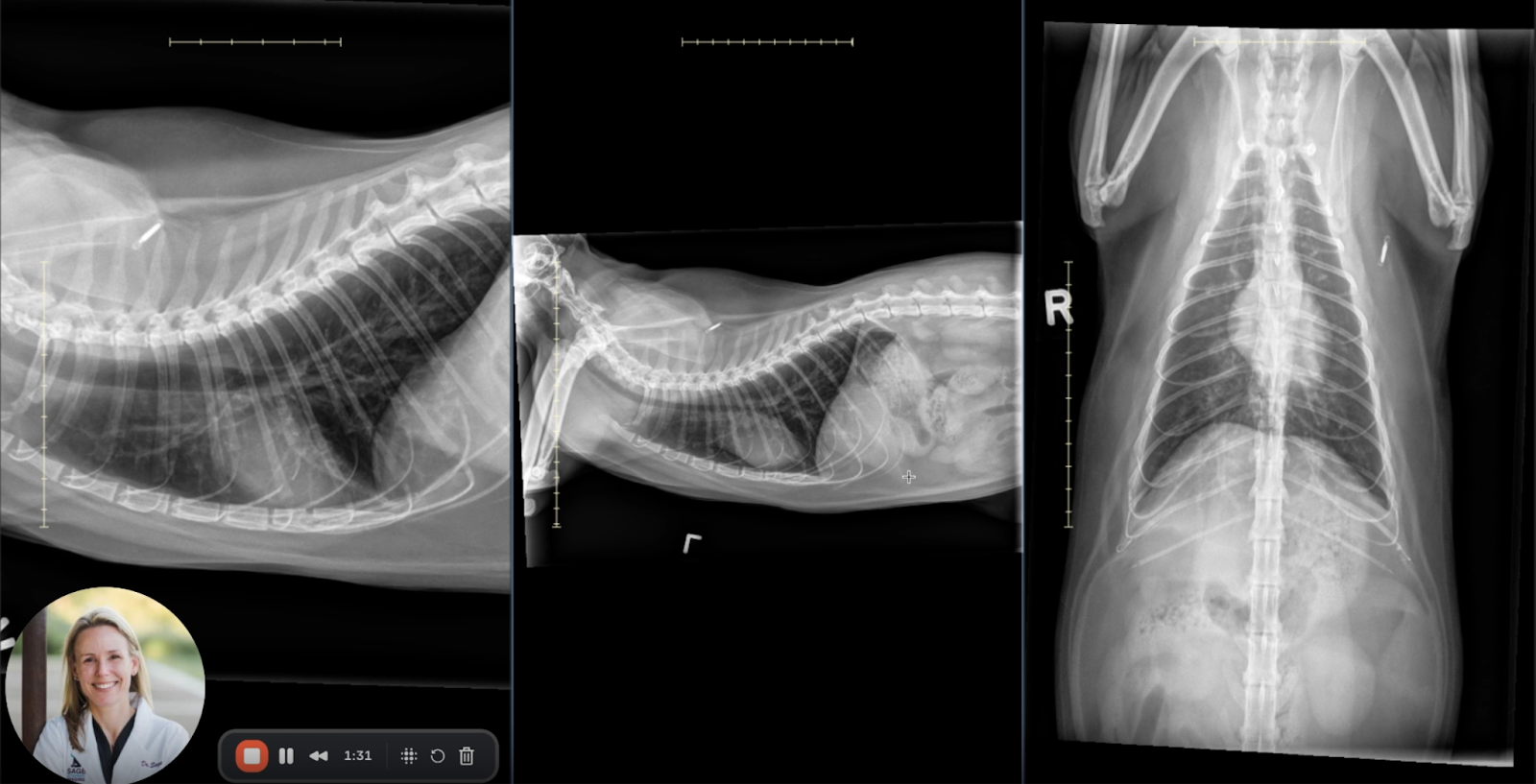
Image 2: Left Lateral View
Bronchial Pattern: Widespread bronchial thickening is confirmed across both cranial and caudal lung lobes. Peribronchial cuffing is visible without evidence of bronchial plugging or alveolar pattern development.
Pulmonary Vasculature: Pulmonary arteries and veins are symmetric and within normal diameter ranges, effectively ruling out pulmonary hypertension or overcirculation.
Cranial Abdomen: The stomach and visualized kidneys are unremarkable, with no evidence of hepatomegaly, masses, or gastrointestinal obstruction.
Image 3: Ventrodorsal (VD) View
Pulmonary Distribution: Bronchial changes are diffuse with no lobar or regional predominance, consistent with a generalized inflammatory process.
Diaphragmatic Configuration: Mild tenting of the diaphragm is observed, further supporting the presence of air trapping and hyperinflation.
Other Findings: No pulmonary masses, nodules, focal alveolar consolidations, or pleural effusion are detected.
Integrated Radiographic Interpretation:
Image 4: Overview
Across all views, the radiographic features are consistent with:
Diffuse bronchial wall thickening (donut and railroad signs)
Pulmonary hyperinflation (flattened diaphragm, increased thoracic volume)
Dilated intrathoracic trachea (indicative of expiratory airflow limitation)
These findings support a diagnosis of chronic lower airway disease (CLAD), with feline asthma being the most probable etiology given the patient's age, clinical signs, and radiographic appearance.
Interpretation and Differentials:
Primary Differential:
Feline Asthma (Allergic Bronchitis)
Characterized by eosinophilic inflammation and reversible bronchoconstriction. Radiographic evidence of bronchial pattern and hyperinflation are consistent with this diagnosis.
Secondary Consideration:
Chronic Bronchitis (Non-eosinophilic/Neutrophilic Predominance)
May share imaging features with asthma but tends to have a more neutrophilic infiltrate on bronchoalveolar lavage (BAL).
Less Likely Differentials:
Parasitic Bronchopneumonopathy
e.g., Aelurostrongylus abstrusus, Toxocara cati, or Toxoplasma gondii
Typically associated with more heterogeneous pulmonary changes, potentially including nodules or alveolar consolidation.
Fungal Pneumonitis
e.g., Histoplasma capsulatum
Generally presents with focal or multifocal soft tissue pulmonary nodules and not uniform hyperinflation.
Educational Notes for Clinical Practice:
Key Radiographic Signs of CLAD:
Bronchial wall thickening with “railroad tracks” and “donut rings”
Pulmonary hyperinflation with flattened diaphragm and tenting
Dilated intrathoracic trachea suggestive of expiratory airflow limitation
Feline Asthma vs Bronchitis:
Both present with similar imaging findings.
Feline asthma typically involves eosinophilic inflammation and bronchoconstriction, while chronic bronchitis may have more neutrophilic cellular infiltrate.
Diagnosis often confirmed with bronchoalveolar lavage (BAL) cytology if imaging is inconclusive.
Follow-Up Recommendations:
Trial of empirical therapy with corticosteroids and bronchodilators.
Consider BAL or tracheal wash if no response or if infectious causes are suspected.
Conclusion:
This case exemplifies classic radiographic indicators of feline chronic lower airway disease. The constellation of diffuse bronchial thickening, tracheal dilation, and pulmonary hyperinflation, in a young, otherwise healthy cat, strongly favors a diagnosis of feline asthma.
While radiography cannot definitively distinguish asthma from chronic bronchitis, it remains an indispensable modality for identifying CLAD and guiding clinical decision-making. Integration with clinical findings and BAL results enhances diagnostic specificity and therapeutic planning.